Baby Brain Research Group
The Baby Brain Research Group studies how newborns' brains get injured and what the best diagnostic tools are to see that injury early on. Our aim is to see brain injury early enough so we can develop treatments to reduce the damage and aid recovery of injured areas. We also hope to identify those children whose long-term development will be affected, and who could benefit from early therapy.
Research
BAMRI Study
The Birth Asphyxia MRI (BAMRI) study implements innovative imaging techniques to assess infants who have encephalopathy in the neonatal period. The study also evaluates the children as they mature to determine the long term effects of neonatal encephalopathy on brain development and neurodevelopmental performance.
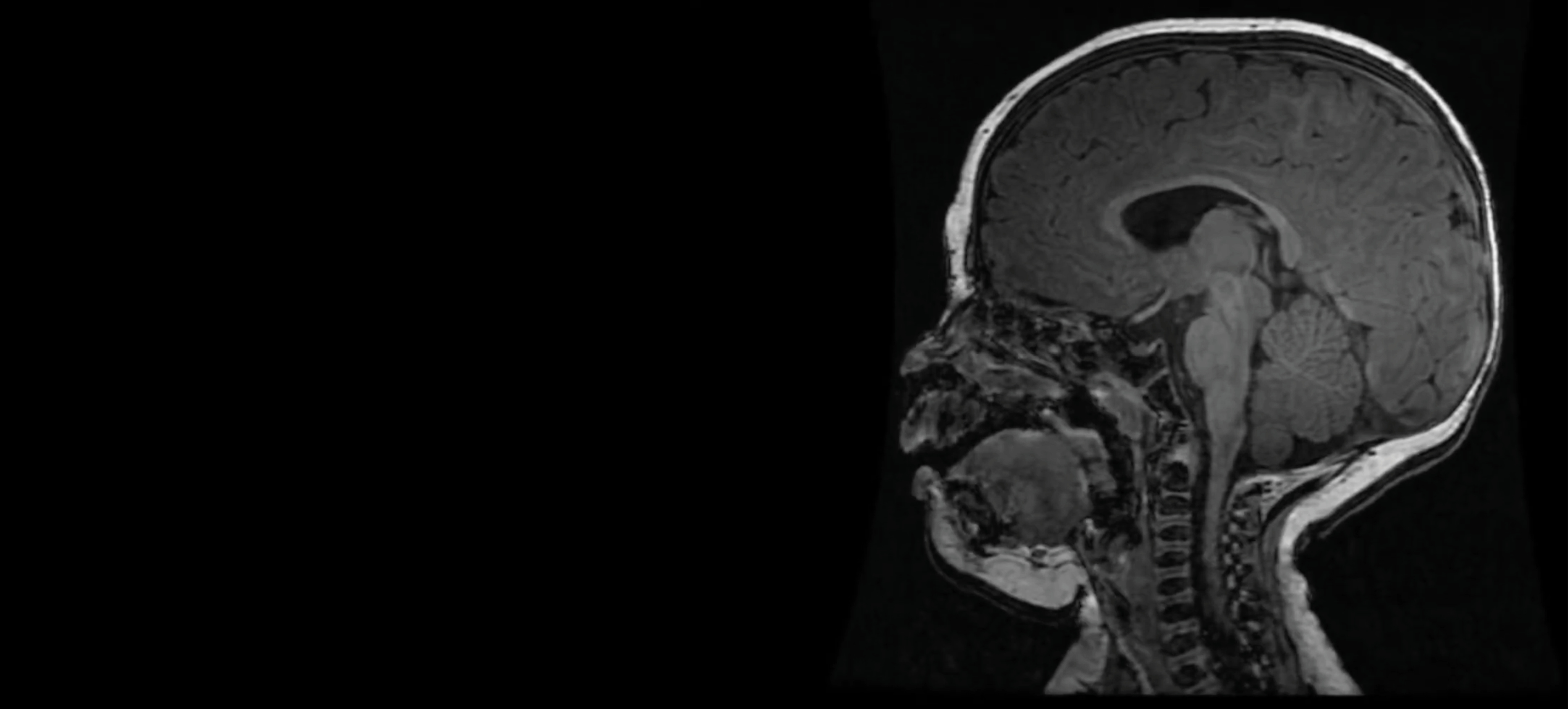
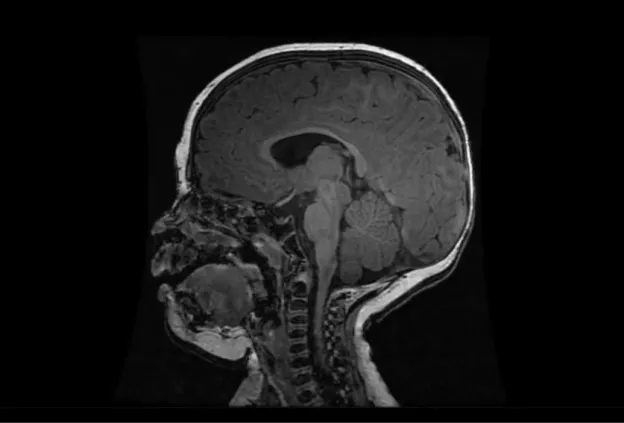
The Birth Asphyxia MRI (BAMRI) project has been ongoing since 1993. The goal was to see how sensitive MRI was in assessing brain injury of babies who had encephalopathy (abnormal neurological exam, seizures, abnormal blood gases) in the neonatal period. We saw that brain injury occurred in certain patterns and were able to conclude that those patterns were associated with specific types of injury. Some types of injuries resulted in damage to areas with high energy demands (brain stem, thalamus, sensorimotor pathways), while others resulted in damage to regions that got less blood flow when blood pressure went down or the heart didn’t contract forcefully. Some babies had damage to the entire brain, presumably due to a long period with essentially no flow to the brain. Still others, had very localized areas of injury, which we call a “stroke” or an infarct. By looking at these patterns of injury and correlating them with outcomes when the babies came back for follow-up neurodevelopmental examinations, our team was able to predict reasonably well what outcome would be based upon the initial MRI.
As time passed, we got additional tools to use on the MRI and more powerful MRIs; these allowed us to do new and better examinations of the babies’ brains. Proton MR spectroscopy (MRS) allowed us to look at effects of the injury on specific chemicals in the brain. Diffusion weighted MR imaging (DWI), which looks at water motion in the brain, could show smaller areas of injury at earlier times and could be quantified to see how bad the injury was in different locations. Even more important, MRS and DWI showed that the injury in the brain rapidly changed over the first few days; it got much worse between day 1 and day 4. This finding was very important, because it taught us that early intervention might reduce the severity of brain injury. This discovery led to the trial of therapeutic hypothermia (TH, also called “brain cooling”). Recent studies have shown that brain cooling significantly reduces brain injury in some newborns, particularly those with injury to the areas with high energy demands when the injury is not very severe. We think that the babies who do not respond well to TH have a different kind of injury, which has progressed beyond the stage where TH is effective. Different therapies are now being formulated and will be used in upcoming trials to see if they are effective.
Overall, the prognosis for newborn babies with encephalopathy has improved greatly over the past 20 years, and the results of BAMRI have contributed significantly to that improvement!
Publications Related to This Study:
PreMRI Study
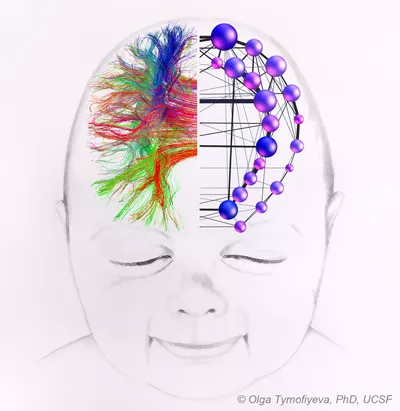
The Prematurely born neonate MRI (PreMRI) study examines the relationship between premature birth, brain injury, and neurologic development using novel imaging techniques developed at UCSF.
The Prematurely born neonate MRI (PreMRI) study has been ongoing since 1998. As with BAMRI, the study has evolved over time. Initially, we were very concerned about transporting such small, delicate babies to the MRI scanner and back. We designed special incubators and transporters to make sure the babies were kept warm and properly monitored during the trip and the MRI; we also had very skilled and careful nurses and doctors who came to the scanners with the babies, ready to act if any problem arose. These incubators and transporters are now becoming commercially available and many more institutions are now doing neonatal scanning.
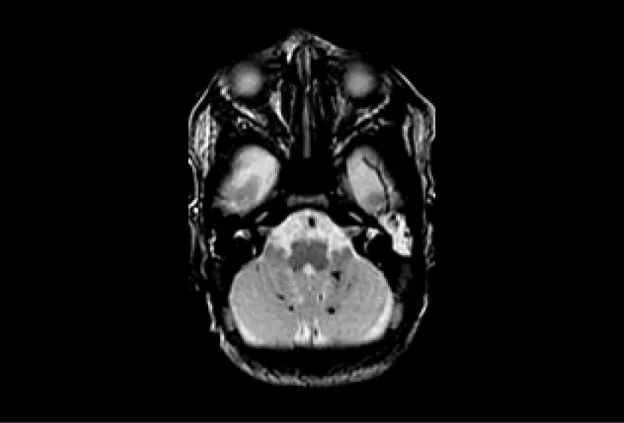
When we first started scanning premature babies, we frequently (>50% of the time) found small abnormalities in the cerebrum. This number has steadily gone down over time, as some of the abnormalities were linked to standard practices that could be changed; now we see cerebral abnormalities in less than 10%. As the cerebral injuries were reduced, our scanners got better and, as a result, we started to see abnormalities in the cerebellum, the smaller, more posterior part of the brain. Over the past decade or so, scientists have begun to realize that the cerebellum is very important in multiple functions of the brain. As we looked closely at the cerebellum, we began to realize that it often had small lesions, as well, and that it was often too small compared to those of babies of the same post-conceptional age who were born at term. Some of this reduced size was a result of treatments that were helping other parts of the baby; these have been altered. We are currently searching for causes of the other small cerebellar lesions and trying to determine if they may be causing the developmental problems that some prematurely born babies manifest. Our ongoing research is focusing on looking at the connections of the cerebellum and cerebrum and trying to determine whether these small cerebellar abnormalities have an effect on cerebral, as well as cerebellar, function.
Cardiac MRI Study
The Cardiac MRI study uses advanced imaging to assess brain injury associated with severe congenital heart disease and its treatments, as well as long term neurodevelopmental outcome of affected children.
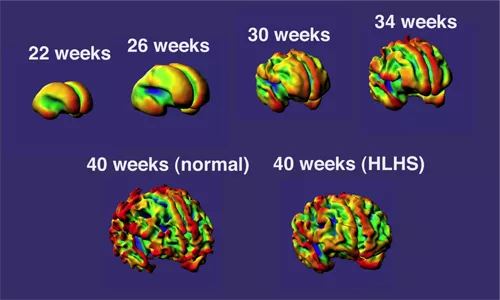
The Cardiac MRI study has been ongoing since 2002. The goal is to understand brain development and risks of brain injury in babies with congenital heart disease. The results so far include:
Newly acquired brain injury is as common BEFORE surgery as after:
This is surprising because prior to this finding many people assumed that the period of greatest risk to the baby occurred during surgery when support with heart/lung bypass is needed to accomplish the repair. Clearly two decades of advances in surgical technique and cardiopulmonary bypass have made surgery safer and more effective! Now our challenge is to extend brain protection into the periods before and after surgery, as well as during surgery.
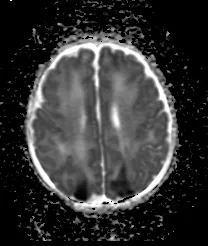
Acquired injuries most commonly take the form of small injuries to the developing white matter:
This observation was very surprising because white matter injury had previously been thought to only occur in newborns born prematurely. This led us to ask the question: ‘Is brain development somehow delayed in newborns with congenital heart disease?’
Brain development is delayed in newborns with congenital heart disease:
This has been the most surprising and influential study result to date. This finding was reported inThe New England Journal of Medicine and led to many newspaper articles and TV coverage. This finding has since been validated by other investigators. Brain development begins to slow prenatally in the third trimester before birth. The delay in brain development is mild (~ equivalent to being born one month premature – e.g. 34-36 weeks instead of 40 weeks gestation). As with premature newborns, evidence suggests that infants with CHD have potential for recovery of developmental milestones as they grow up, with improvements noted during infancy and childhood as they are followed with repeated testing.
Moderate to severe white matter injury predicts motor impairment in infancy:
This is our most recent publication in the Journal of American College of Cardiology and has been influential in changing clinical practice for our babies with congenital heart disease. For the first time, our study demonstrates the benefits in obtaining brain MRI in the newborn period in order to identify the highest-risk patients for neurodevelopmental impairment.
Publications and presentations related to this study:
- Temporal and Anatomic Risk Profile of Brain Injury with Neonatal Repair of Congenital Heart Defects (pdf)
- Abnormal Brain Development in Newborns with CHD (pdf)
- Clinically Silent Preoperative Brain Injuries Do not Worsen with Surgery in Newborns with CHD (pdf)
- Association of Prenatal Diagnosis of Critical CHD with Postnatal Brain Development and the Risk of Brain Injury (pdf)
- Neonatal Brain Injury and Timing of Neurodevelopmental Assessment in Patients with CHD (pdf)
- The Neonatal Brain in Critical CHD (pdf)
- Neurodevelopment in CHD: Brain Imaging & Optimizing Outcomes (Video)
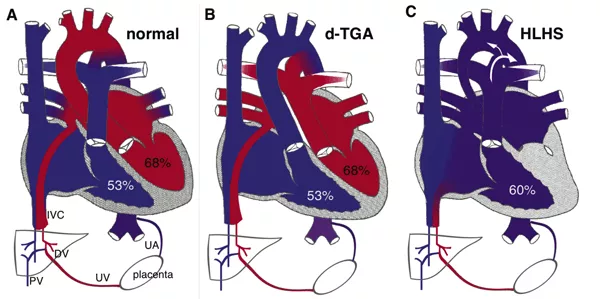
Currently we hypothesize that delayed brain development may put newborns with CHD at risk of white matter injury around the time of surgery. ‘White matter’ includes the connection between brain cells (neurons or ‘grey matter’) and the cells that produce ‘myelin’ to support and insulate the neurons. We are focused on identifying interventions or medications to prevent any brain injury around surgery. Selecting these interventions would not be possible without the information we have gathered from our study babies to date.
We are finding that children with heart disease repaired during infancy, share many aspects of behavior and learning styles noted at school age in children born prematurely. Both groups score within the normal range on IQ testing, but are challenged by tasks that require attention, executive function and visual-motor integration.
Our present focus includes fetal MRI to understand how brain development is affected by congenital heart disease before birth. We are also following infants and children after surgery to watch how they develop into school age and beyond to understand and achieve optimal brain development, or if needed, repair and recovery following newborn heart surgery.
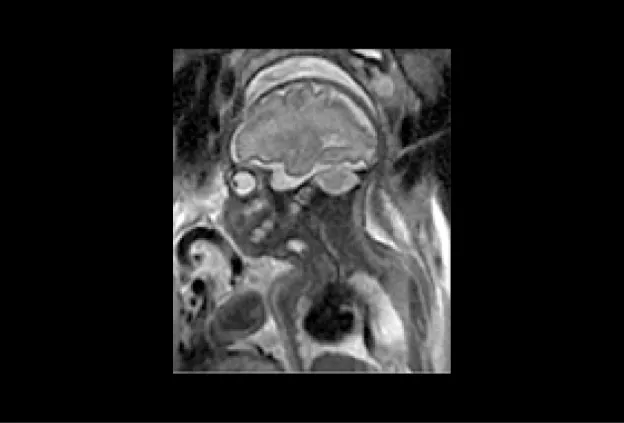
Fetal MRI Study
The Fetal MRI study is developing methods to better assess and quantify development of the nervous system in the fetus, thereby allowing early detection of developmental abnormalities. In addition, the study is comparing how accurately fetal MRI detects changes in the fetus’ brain and spine during pregnancy compared to ultrasound.
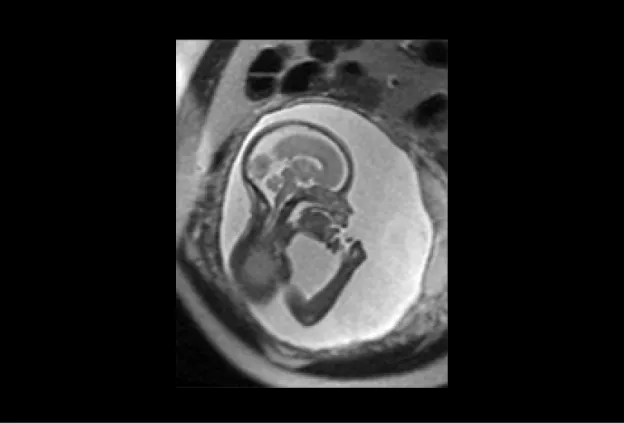
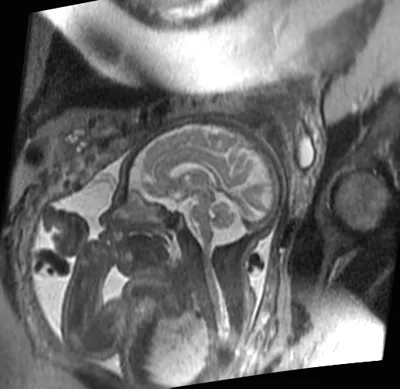
UCSF is one of the few sites in the country that is experienced with performing and interpreting fetal MRI. We have performed fetal MRI since 1996. The findings from our fetal MRI study will help us provide pregnant women with the most advanced and accurate information during their pregnancy.
First, we would like to see how accurately fetal MRI detects changes in the fetus’ brain and spine during pregnancy compared to ultrasound. While ultrasound is the most commonly used method of monitoring fetal development, its ability to detect changes in the brain is limited. In this study, we are comparing ultrasound and MR images of fetuses to identify the situations in which fetal MRI will provide valuable clinical information not seen on ultrasound. Studies have shown that, overall, fetal MRI is more helpful than ultrasound in evaluating the brain. We are interested in studying just how helpful fetal MRI is for different brain conditions.
Second, we would like to learn how various congenital (inherited) and acquired abnormalities detected on fetal MRI correlate with childhood development. Currently, it is very difficult to counsel parents who have a fetus with a brain abnormality, because outcomes can vary widely. By classifying abnormalities more thoroughly with fetal MRI, we will be able to give parents a more accurate picture of what they can expect for their child from a neurological and developmental standpoint. This information will help parents make decisions during pregnancy and prepare in advance for challenges their child and family may face.
Since developmental outcome is a crucial aspect of our study, it is very important that we keep in touch with your family as you make decisions about your pregnancy and, if your child is born, throughout his/her early years.
If your fetus has a condition known as Isolated Mild Ventriculomegaly, we are no longer accepting new patients for this study and will not be offering a second fetal MRI for free. If you have already enrolled in our study on Isolated Mild Ventriculomegaly, then we will contact you to schedule the neurological and developmental assessments after your child has been born.
Contact Us
Baby Brain Research Group
For information on BAMRI, PreMRI, or Cardiac MRI studies, contact:
Laurel Haeusslein
Lead Clinical Research Coordinator
Ph: (415) 476-9737
Laurel.Haeusslein@ucsf.edu
Veronica De Santiago
Study Coordinator
Ph: (415) 476-8717
deSantiagoV@peds.ucsf.edu
Onika Chambers
Study Coordinator
Ph: (415) 476-9737
Onika.Chambers@ucsf.edu
For information on Fetal MRI studies, contact:
Orit Glenn, MD
Professor
Ph: (415) 353-2526
orit.glenn@ucsf.edu
505 Parnassus Ave, Room M793
San Francisco, CA 94143-0114
Toll Free Phone: 1 (855) 582-2229