Read about our preliminary results in this UCSF Radiology Blog post!
Low bone mineral density (BMD) and increased fracture risk are increasingly recognized as significant sequelae of HIV infection and treatment. As HIV-infected individuals live longer through effective antiretroviral therapy (ART), HIV-related bone loss is superimposed upon age-related bone loss, resulting in up to 4-fold higher annual rates of fragility fracture in HIV-infected individuals than in the general population. The pathophysiology underlying skeletal changes in the setting of HIV infection appears to differ from that of non-HIV populations experiencing osteoporosis. For example, low BMD does not explain increased fracture risk in HIV-infected individuals. An emerging explanation for this paradox is that HIV infection is associated with bone quality changes – specifically in bone geometry and microstructure – that do not impact BMD but do increase fracture risk. The etiology of these bone quality changes is unknown. Our hypothesis is that, as in non-HIV-infected populations with low BMD, preferential differentiation of adipocytes over osteoblasts results in increased marrow adiposity and associated decreased bone quality.
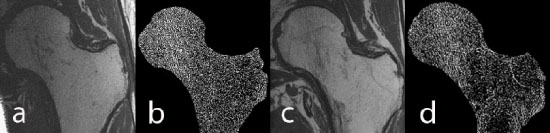
The aim of this project to apply novel high-resolution image acquisition and analysis to:
- Quantify bone quality deterioration in HIV-infected patients relative to uninfected controls, and
- Determine the relationship between marrow adiposity and bone quality deterioration in HIV-infected patients.
Funded by NIH/NIAID R01 AI125080